Low back pain one of the leading cause for Years of healthy life lost due to disability (YLD). Low back pain can be a drain on the pocket of the patient from treatment expense (including a free dose of radiation, useless MRI and PT ) to absenteeism.
Classification system abound
If you, like me, have studied manual therapy, you'd likely have been mesmerised by the complicated way a manual therapist diagnosis and classification of patients with LBP. You know from the facet syndromes to the all pervasive disc bulge. And to add to confusion everyone who writes a manual therapy book has a different ways of classification. The no one can teach McKenzie Method has 3 syndromes, the trigger point boys are frequentist- they count the hell out of the tender points, the imbalance guys have cross syndromes, the x-ray and MRI boys have L 4 L5, then- well you get the point.
The funny point is everyone publishes studies to show there method is reliable. This leaves one questioning: how can all these methods claim to be reliable, and if they are all reliable, which among them yields the best outcomes?
What does it all mean?
The purpose of a classification system is to prescribe appropriate treatment based on the classification and facilitate quicker based recovery compared to approaches without such classification. It should ideally result in reduced expenses for both the healthcare system and patients. Unfortunately, no system has yet demonstrated clear superiority. From methods like the McKenzie technique to focusing on L4 L5 degeneration, none have shown definitive advantages. They all seem akin to horoscopes predicting whom to marry— whatever the soothsayer says- you are doomed, i mean you are going to be married.
What is the better way?
Among the myriad classification systems, the most straightforward approach involves triaging patients into three primary types:
Red flags: These indicate emergent pathologies that require immediate attention.
Non-specific low back pain: Denotes back pain with causes that are difficult to determine or specify.
Sciatica (radiculopathy): Specifically referencing pain originating from the compression of spinal nerve roots, often manifesting as radiating pain from the lower back down the leg.
How to do it?
Identifying red flags: Well, it is fairly simple. When any patients come to you clinic with back pain- the first step is to rule out if the patient has systemic disease. That is is the pain in the back due to disease from other systems like space occupying lesions, kidney stone, fracture of the vertebrae and many more. If you suspect and in your mind there is a .1 percent chance there can be a emerging pathology- refer to appropriate consultant (there is no wait and watch). This evaluation primarily relies on meticulous history-taking, detailed in good books and reviews. While not foolproof, it serves as a practical method in clinical practice.
Identifying Non-Specific Low Back Pain: Once systemic diseases are ruled out, we have to assume all the patients are having back pain due to unknown reason- non-specific low back pain. No further sub-classification is pursued at this stage.
Identifying Sciatica: For patients experiencing radiating pain with sensory and motor weakness, the likelihood of sciatica is higher. When diagnosing sciatica, it's important to bear in mind two critical points:
It's relatively uncommon.
The patient should exhibit nerve pain (distinct from other types of pain) along with symptoms of radiculopathy.
What’s the advantage of this system?
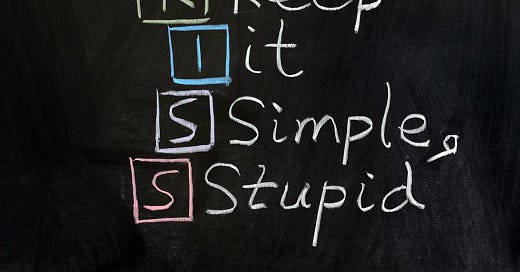
Well, it is fairly simple, and does not unnecessarily complicate things. It reduces the need for expensive photographs of the spine, vitamin D test and host of other “tests”. It is better than any other complicated classification methods in reducing the burden of low back pain- financially and reducing disability.
This is not a new radical method. It is been there for decades, just that we think using complicated things is intelligent. But as we know the intelligent thing is what helps the patient best not what makes us look “rad”.